It’s widely reported that young people are facing severe mental health issues resulting from the pandemic, years of social unrest, and traumatic violence. To understand the gravity of the mental health crisis facing Chicago’s youth, the non-profit organization Youth Outreach Service (YOS) has released data from its assessments of its services.
The number of at-risk youth seeking help from YOS for mental health issues more than doubled when students returned to in-person learning last fall. And mental health referrals have skyrocketed since then. Chicago’s young people struggle with a variety of mental health concerns including anxiety, depression, behavioral challenges in and out of school, suicidal thoughts, and others.
The pandemic worsened youths’ mental health crisis
The pandemic has undoubtedly aggravated the situation. According to a survey carried out by Anne and Robert H. Lurie Children’s Hospital in Chicago and covered by NBC News, 44% of young children and youth in Chicago have shown an increase in symptoms of behavioral or mental health issues during the COVID-19 pandemic.
Though masks continue to come off in Chicago and across Illinois, the impact of the pandemic’s unprecedented life disruption, isolation, and other effects lingers, taking a huge toll on our young people.
Watching an otherwise healthy and happy child struggle with mental health issues is heart-wrenching. Many of Chicago’s guardians, parents, and other stakeholders know this feeling too well. Now more than two years into the pandemic and already trying to cope with increases in violence and social and political unrest, our youth are in serious pain.
Rates of depression, hopelessness, sadness,
And anxiety has skyrocketed among children so quickly that several institutions – including the American Academy of Pediatrics, American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association – have declared a national state of emergency. The U.S. Surgeon General followed suit at the end of last year, issuing an urgent public health advisory on youth’s mental health crisis.
School counselors report spikes in behavior challenges, violence, and mental issues in their learning institutions, and therapists report long waiting lists for help. Emergency department clinicians and healthcare providers are overwhelmed by the number of children and youth coming in for various mental health emergencies, ranging from self-harm to suicide attempts. Worse, there’s a dire shortage of behavioral and mental health providers in Illinois, making it harder for parents and youth to find help.
Of course, the problem isn’t specific to Chicago and Illinois. According to CNN coverage, the whole nation is in the midst of an unprecedented mental health crisis among America’s youth, and there are concerning indications that it may get worse before it gets better. Clearly, our youth are crying out for help – but do we hear them?
Help on the way
With mental health issues increasing among hospital patients, new solutions are coming to help. One such example is the upcoming Geode Health practice in West Loop, Chicago, which will offer therapy services for all ages.
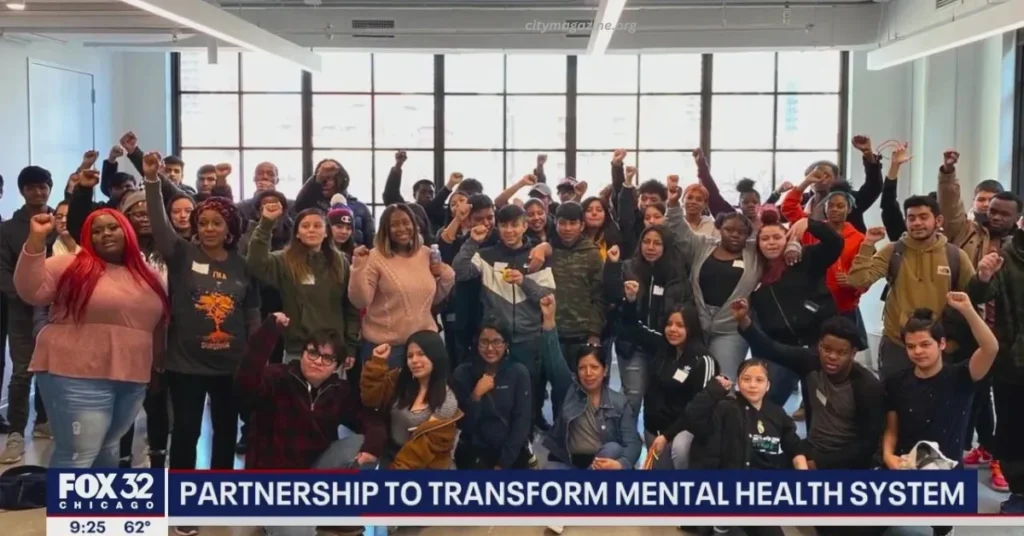
In addition, the federal government, state officials, concerned non-profits, and other stakeholders have vowed to tackle the issues head-on. Recently, the Center for Childhood Resilience (CCR) at Lurie Children’s Hospital of Chicago and the Chicago Public Schools (CPS) began ramping up their collaborative efforts to support youth mental health in the city.
CPS and CCR are expanding their collaborative and comprehensive system to better detect mental health issues among Pre-K-12 students, as well as provide timely response and support. The program will grow from just covering 200 pilot schools within the Chicago Public Schools to expanding to all district schools. The main goal is to boost the school district’s intervention efforts for the burgeoning mental crisis among Chicago’s youth.
The school-based Behavioral Health Team
(BHT) model will help optimize resource use and collaboration efforts between CCR and CPS. In addition, the model will be used to identify students with behavioral and mental health needs so they can be quickly connected to evidence-based help. The BHT is the brainchild of a group comprising mental health providers, educators, and other key players from CPS and CCR at Lurie Children’s Hospital.
The BHT model has already been active in 200 pilot schools under the CPS umbrella and, going forward will cover all 515 CPS network schools. They won’t stop there, though. The program director says it plans to expand the BHT model to all schools in the region by the 2023/24 school calendar year. Expanding the trauma-based BHT efforts is part of the Chicago Public Schools District’s Healing-Centered Framework. It will be implemented under the recently ratified Comprehensive Mental Health and Suicide Prevention Policy.
Although the ultimate budget for the complete expansion of the program is still in the pipeline, CPS plans to use funds from various sources to finance the expansion in the School Year 2023. One such important source is the federal COVID-19 relief funds. The journal Psychology in Schools recently spotlighted the implementation and feasibility study of the BHT model by psychologist Tali Raviv, an Associate Professor of Psychiatry and Behavioral Sciences at Northwestern University and the Associate Director at the Center for Childhood Resilience at Lurie Children’s Hospital.
Wrapping It Up
The youth mental health crisis is a growing concern for Chicago’s parents, educators, and other stakeholders. The expansion of the BHT will significantly increase support when it comes to detecting mental health issues among young people and providing appropriate referral services. The targeted mental problems range from depression, anxiety, and other trauma-related symptoms to substance abuse and disruptive behavior. With greater help available, children’s relief from the pain of the last few years is in sight.